A 5 part series – Understanding the different types of pain allows the individual to recognize the best plan of action for medicine, therapy and treatment. As every person is unique, treatment plans should include the option for alternative therapies, such as medicating with cannabis, to manage chronic pain.
- Part I – The Characterization of Pain
- Part II – The Endocannabinoid System
- Part III – Contrasting Approaches for Pain Management
- Part IV – Medical Cannabis Use for Chronic Pain
- Part V – Medical Cannabis for Opioid Reduction
Part I – The Characterization of Pain
Acute pain is the type of pain that typically lasts less than 3-6 months, is directly related to soft tissue damage and gradually resolves as the tissue heals. Examples include: paper cuts, ankle sprain or labor pains.
Chronic pain, on the other hand, is different in that the pain persists for more than 6 months and can take a toll on your day-to-day life and mental well-being. Examples include: osteoarthritis, multiple sclerosis, or fibromyalgia. All forms of pain are produced in the brain. Chronic pain is pain that is still being produced after your body has healed. Ongoing pain is less about structural changes in the body and more about the sensitivity of the nervous system generating the chronic pain. Looking at persistent pain from a broad perspective with a structured approach in developing a plan to utilize a multi model approach to alternative and medical treatment may be helpful.

- The Endocannabinoid System can regulate the 8 types of pain:
- Acute: Resulting from a small injury, usually self-correcting in a few days/weeks
- Chronic: Long term pain (lasting longer than 3-6 months)
- Central: Neuropathic pain generated in the central nervous system
- Peripheral: Neuropathic pain in the extremities and peripheral nervous system
- Noxious: Caused by the stimulation of nociceptors, which are the pain receptors for tissue injury.
- Inflammatory: Increased sensitivity due to inflammatory response associated with tissue damage.
- Pathological: Characterized by an amplified response to normally innocuous stimuli and an amplified response to acute pain.
- Mental/emotional: Suffering due to non-physical/psychological stimuli
From the perspective of others, pain may be visibly noticeable, yet many forms of pain remain invisible to others. Pain can be neuropathic such as diabetic neuropathy or acute pain from pricking a finger to test blood glucose levels. Pain can be profound flareups and felt systemically, like rheumatoid arthritis or osteoarthritis. Pain can also be the heart-wrenching sadness, grief and ache of loosing a loved one and the invisible pain of traumatic events. With seemingly limitless numbers of variables contributing to pain, it is helpful to take notes to understand your individual journey of pain management. Take note of:
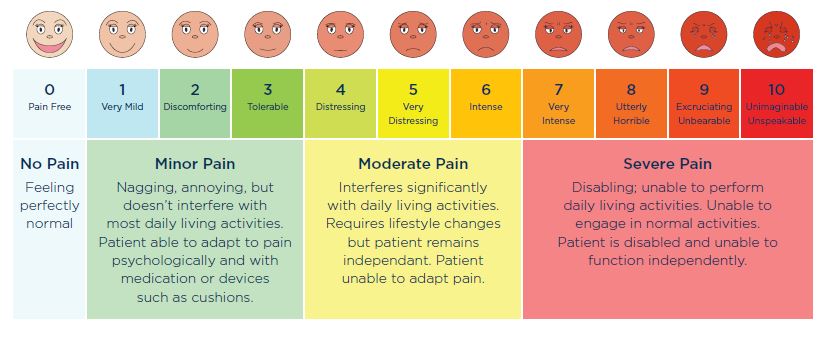
- Pain Intensity Levels – Is it mild, moderate or severe? Use the Pain Scale
- Time Course – When did your injury occur? Is your pain acute or chronic?
- Tissue Types – What tissues type is involved where your pain is felt? Is your pain felt in your skin? Muscles? Viscera, joints, tendons, or bones?
- Syndromes – Do you have any syndromes or pertinent signals of pain, such as cancer, fibromyalgia or migraines.
- Additional Factors – How is your psychological and behavioral state? How does your age, gender, diet and culture play a role in your overall health, impact on pain and practices for pain management?
As pain is dynamic, it is a good idea to keep a journal – logging your pain, the intensity, time of injury or flareup and duration of time. Take note on how you are managing your pain, the type of medication you take, and your personal inventory of how you feel after taking pain medication. As each individuals life journey is unique, taking these measurements can help to manage pain by knowing what you feel, how you’ve managed it and its effects so you can clearly communicate the details with a physician to start the road to recovery.
Remember to talk to your primary care physician about your pain and connect with a certifying cannabis physician to learn how medical cannabis may be the best choice to manage your chronic pain.
Part II – The Endocannabinoid System
Did you know, all vertebrates have an Endocannainoid system? The Endocannabinoid System, or the ECS, is a physiological system made up of neurons, cannabinoids, and cannabinoid receptors throughout our body. Cannabinoids are chemical compounds produced naturally within the body or from substances produced to mimic the effects of natural cannabinoids. Let’s break this definition down one step further.
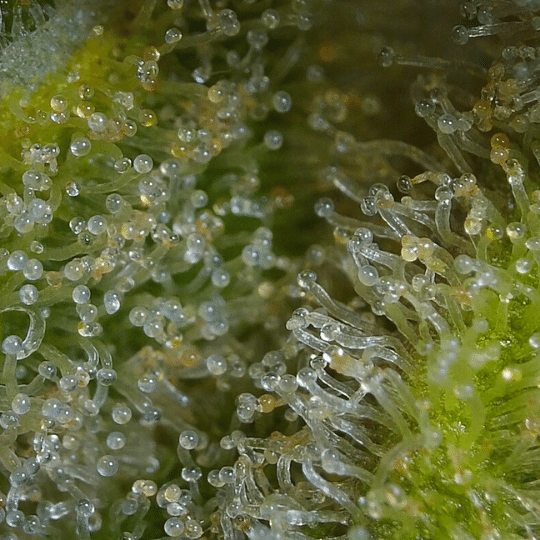
Endocannabinoids are cannabinoids made within the body, where Endo – means “inner”. The two primary compounds our bodies produce are Anadamide (AEA) and 2-Arachidonoylglycerol (2-AG), where Ananda – is Sanskrit for “bliss”. Phytocannabinoids are cannabinoids produced by cannabis (Phyto – meaning “plant”). These compounds include THC, CBD, CBN, CBDA, CBG, THCV, THCA, etc. The purpose of the Endocannabinoids System is to unlock and bind with specific receptors to regulate the functions in the body to maintain optimal health or homeostasis. The exact layout of each person’s ECS is unique, which is why cannabis affects each of us differently. All vertebrates are born with an Endocannabinoid System
The Endocannabinoid System consists of three parts: receptors, cannabinoids and enzymes. A complex network of cannabinoid receptors are located on the surfaces of cells throughout the body. Endo or Phyto Cannabinoids are molecules that bind to and “activate” the receptor sites. Enzymes are molecules that break down the cannabinoids after they’re used and build receptors when necessary. Cannabinoids are the ‘keys’ within our Endocannabinoid System that fit into specific ‘locks’ or receptors, to balance our bodily functions.
- Receptors
- The quantity and quality of receptors determine the sensitivity to cannabinoids.
- Researchers have found that small doses of cannabinoids can signal the body to build more receptors. This is why cannabis tends to be more effective after your first experience.
- Each type of receptor is designed to bind to only one type of cannabinoid, making this system extremely effective.
- CB1 and CB2 receptors are the most common types of receptors
- Cannabinoids
- Endo’ or ‘Phyto’ cannabinoids
- Cannabinoids bind to the receptors to activate them, causing a chain reaction to regulate the body function.
- Cannabinoids are unique because they travel both ways between neurons telling the body when to begin and stop a process.
- Metabolic Enzymes
- The enzymes are builders and clean-up
- The ECS crew, the 2 main enzymes are:
- FAAH which breaks down Anadamide
- MAGL which breaks down 2-AG
The Endocannabinoid System is responsible for balancing many processes, including controlling the stimulation of nerve cells to increase or decrease pain. The Endocannabinoid System regulates brain cell firing, known as Neural Firing. If a neuron in the brain is mis-firing or overactive, it can create a sensation of pain where there is no injury. If a cannabinoid is introduced to the system, it will bind to that neurons CB1 receptor where a signal is then transmitted to the neuron that instructs it to reduce it’s firing.
When the immune system is activated for too long it results in chronic inflammation. This can end up affecting healthy tissues resulting in autoimmune disease. Research shows that cannabinoids have anti-inflammatory effects when introduced at the sight of injury.
Part III – Contrasting Approaches for Pain Management
What tools are helpful for communicating your level of pain and how you feel? There are a few approaches to assess pain. The classic model is the Comparative Pain Scale Chart. You may have heard a physician ask this before, “On a scale from 1 to 10, with 10 being the worst, how would you rate your pain?”
The Pain Scale is a tool medical professionals use to assess an individual’s pain. Pain scales are used at regular doctors visits, before surgery, after surgery, and when self-reported injuries occurs. Only patients can describe characteristics and rate the severity of their pain. Physicians use the pain scale to better understand a persons pain, taking note of the duration, severity and type which helps them prescribe the best treatment for the type of pain.
The World Health Organization (WHO) recommends physicians use the Three-step Pain Ladder, which has been widely used by physicians since 1986 – a model that is 34 years old! Physicians use the pain scale, patient history and Three-step Pain Ladder to make an accurate diagnosis, create a treatment plan, and measure the effectiveness of the treatment. Why limit the treatments to opioids and pharmaceuticals?
As every person is unique, a one size fits all model for treating pain is an outdated approach, especially at a time that the country is facing an opioid epidemic. Treatment therapies solely focusing on pharmaceuticals and opioids are limiting and perpetuate the abuse of addictive, toxic prescriptions.
New models to treat pain have been analyzed, including the multi-modal approach to pain treatment therapies. Alternative therapies, such as medical cannabis (cannabinoids), acupuncture, and physical therapy, provide a broader approach to adopt tailor made therapies unique to the individual. The “trolley analgesic model” includes western transitional medicine, but also includes medical cannabis as a non-toxic alternative with success for treating chronic pain. Always consider using alternative approaches when necessary.
Part IV – Medical Cannabis Use for Chronic Pain
Cannabis is medicine as it contains phytocannabinoids – plant derived organic compounds containing pharmacological properties that bind with receptors to provide systemic homeostasis. With over 500 compounds, including over 100 different cannabinoids, cannabis helps to regulate chronic pain by binding with the receptors to mimic internally produced endocannabinoids. The most prevalent phytocannabinoids are Cannabidiol (CBD) and Delta-9 Tetrahydrocannabinol (THC). CBD is known for being non-intoxicating as it does not provide a “high” feeling. It changes the brain and body chemistry to provide anxiolytic, antispasmodic, anticonvulsant, and anti-inflammatory relief. CBD is also known to offer neuropathic pain relief. In fact, the United States Government holds patent #6630507 stating CBD has antioxidant and neuroprotective properties, yet the plant is still classified as a Schedule 1 substance. Like CBD, THC is beneficial for specific types of chronic pain. Known for its “intoxicating” effect, THC produces medical effects to promote sleep, muscle relaxation, appetite stimulation, with analgesic properties equating to “opiate type pain relief.”
One of the most common qualifying conditions for medical cannabis in Massachusetts and the nation is relief from chronic pain. One study reported that 87 percent of medical cardholders, in Colorado, were seeking chronic pain relief through cannabis. In 2017, the National Academy of Sciences published The Health Effects of Cannabis and Cannabinoids, which analyzed the current state of scientific evidence, with references and discussions for future research. One study evaluated the effects of inhaled cannabis on pain management and found that cannabinoids reduced pain by approximately 40% compared to the controlled condition. In another study, researchers compared the influence of inhaled cannabis on HIV neuropathic pain in a randomized placebo-controlled trial. Of the group, smoking cannabis reduced daily pain by 34% and 17% in the placebo group. A reduction greater than 30% was reported by 52% in the cannabis group and half that in the placebo group. In addition, the first cannabis cigarettes reduced chronic pain by a median of 72% and by 15% in the placebo group.
Smoking cannabis effectively relieves chronic pain, including neuropathic pain, however the method of cannabis administration influences the length of medicinal effect. Many patients seeking chronic pain relief are resorting to medicated tinctures and edibles as they provide a longer duration (4 – 8 hours) compared to cannabis inhalation or vaporization (1 – 3 hours). This is an important factor when patients express difficulty sleeping due to pain discomfort. Edibles are helpful for a long duration while inhalation provides immediate symptom relief. Patients who struggle with localized pain also use topicals, such as infused salves or creams, for targeted treatment without intoxication. Supported through scientific research, there is substantial evidence that cannabis is an effective treatment for chronic pain as it continues to help the medical community relieve symptoms.
Part V – Medical Cannabis for Opioid Reduction
With over half a million drug overdose deaths from 2010 – 2020, pharmaceutical prescription overdoses continue to contribute to mortality in the United States. Although no one predicted the ferocity of this opioid epidemic, the fragmentation is tied to the prohibition of cannabis as medicine with pharmaceutical giants profiting from western medicine. (Click here to check out our blog post on The History of Medical Cannabis in the United States.) Cannabis has been used as medicine for hundreds of centuries, yet since its prohibition, western medicines recommendations became the only option for pain management. Opioids are a class of drugs that include pharmaceuticals (such as oxycodone, hydrocodone, codeine, morphine, and others), the illegal drug heroin, and synthetic opioids such as fentanyl. Opioids work by binding and activating the opioid receptors on cells throughout the body, especially those involved in feelings of pain and pleasure. When opioids bind to these receptors, they block pain signals and release large amounts of dopamine. This release strongly reinforces the act of taking the drug, making it addictive.

Opioids are dangerous for long term chronic pain management as they cause the sensation of pain to increase overtime. They provide relief by blocking pain, yet the body reacts by increasing the number of receptors to try to get the pain signal through. When the drug effects wear off, the person experiences more pain. Taking more opioids becomes less and less effective as the pain keeps increasing due to the opioids themselves and not because of the initial injury.
Cannabis may be useful in the treatment of opioid reduction as cannabinoids provide pain relief through similar signals. The Endocannabinoid System modulates the reward circuitry in the brain that is linked to drug addiction to allow room for cannabinoid recovery. One study found THC can reduce the amount of opioid needed to treat pain, which may be helpful in reducing both opioid dependency and overdoses. The Endocannabinoid System regulates the body’s response to reward and stress, which helps its role in combatting drug abuse and addiction. Cannabinoids interfere with fundamental neural mechanisms underlying drug-use reward, drug-seeking compulsive behaviors, and anxiety related to both addiction and relapse.
In 2017, Cannabis and Pain: A Clinical Review was published by the National Institute of Health showing evidence supporting the use of cannabis pharmacotherapy for certain clinical scenarios. Multiple findings suggest a potential role exists for medical cannabis in pain management, although research shows varied effectiveness depending on the type of pain. Moreover, the co-administration of cannabis with opioids may result in reduced opioid requirements. The National Academies of Sciences, Engineering and Medicine published, in 2017 research on The Health Effects of Cannabis and Cannabinoids: Current State of Evidence and Recommendations for Research showing substantial evidence that cannabinoids are effective for the treatment of pain in adults which allows many patients to reduce or even eliminate opiate use. One study found patients with chronic pain enrolled in state’s medical cannabis program were found to be 83% more likely to reduce daily opioid prescription dosages or 40% more likely to cease filling the prescriptions altogether. Cannabis pharmacology has been so effective in addressing the opioid epidemic that cannabinoids are even part of the NIH strategic initiative to address the opioid crisis. In addition, research shows medical cannabis laws are associated with lower opioid overdose deaths. Between 1999-2010 states with medical cannabis laws had a 24.8% lower mean annual opioid overdose mortality rate compared to states without medical cannabis laws.
Cannabis has been used as medicine for centuries with no record of human overdose using safe sources. Although the United States wrongfully classifies cannabis as a Schedule I substance with no medical potential, there is significant information supporting it as such. In this pivotal time of US history, cannabis must be descheduled and studied in clinical studies for its pharmacological properties. Medical cannabis may be the exit drug the world needs from addictive, harmful pharmaceuticals and an alternative treatment for those struggling with chronic pain.
Talk to your primary care physician about your medical health and connect with a certifying cannabis physician or nurse practitioner, here, to learn how medical cannabis may work for you.
Want to stay informed of special promotions, events, and cannabis education? Click here to sign up for the monthly newsletter.